What is a Pelvic Organ Prolapse?
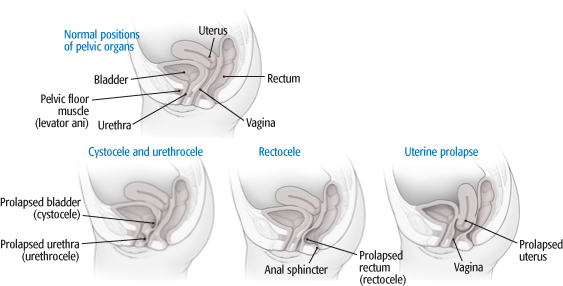
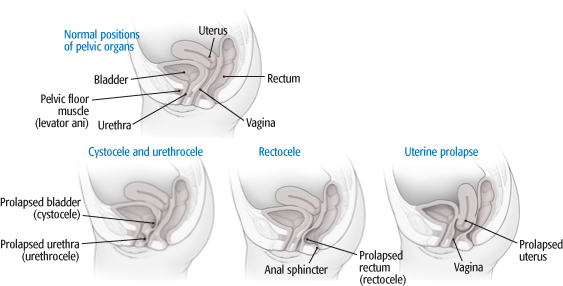
In some instances, the bladder can drop below the supportive anterior vaginal wall which is called a cystocele. In other cases, the rectal wall can also bulge above the supportive rectal vaginal wall which is referred to as a rectocele.
At other times, a prolapsed uterus occurs. This is when all of the pelvic organs including the uterus or the upper portion of the vagina can protrude down into lower portion of the vagina or even outside of the opening of the vagina.
Overview of Symptoms
- Pressure or fullness in the pelvic area
- Painful intercourse
- A feeling that something is falling out of the vagina
- Leaking of urine
- Chronic urge to urinate
Overview of Treatment Options
- Pelvic floor physical therapy to strengthen weakened muscles
- Robotic prolapse surgery, including a cystocele repair or rectocele repair
CLICK HERE to contact us using our live chat for more information on treating a prolapsed uterus or to schedule an appointment to discuss your options and get the process started so you can have relief as soon as possible!
If you have pain and discomfort from pelvic organ prolapse that does not respond to nonsurgical treatment and lifestyle changes, you may want to consider surgery. The choice of surgery depends upon which organs are involved, how bad your symptoms are, and what other medical conditions are present.
Types of pelvic organ prolapse:
Different types of pelvic organ prolapse affect different parts of the vagina (see illustrations):
- Cystocele and urethrocele. A cystocele occurs when the bladder protrudes into the front wall of the vagina. A similar defect, known as a urethrocele, develops when the urethra presses into the front vaginal wall.
- Rectocele. Part of the rectum bulges into the back wall of the vagina, sometimes causing difficulty with defecation.
- Uterine prolapse. The uterus drops down into the vagina. In women who have undergone a hysterectomy, a similar condition known as vaginal vault prolapse can occur: the top of the vagina protrudes into the lower vagina.
What causes pelvic organ prolapse?
Pelvic support comes from pelvic floor muscles, connecting tissue (fascia), and thickened pieces of fascia that serve as ligaments. When pelvic floor muscles are weakened, the fascia and ligaments have to bear the brunt of the weight. Eventually, they may stretch and fail, allowing pelvic organs to drop and press into the vaginal wall.
Women who have had multiple vaginal births are at greatest risk for pelvic organ prolapse, particularly after menopause. Other risk factors include surgery to the pelvic floor, connective tissue disorders, and obesity.
What are the symptoms?
Women with mild prolapse discovered during a routine pelvic exam may have no symptoms at all. But others experience considerable discomfort and a range of symptoms, including:
- Pressure and pain. The most common complaints are a feeling of pelvic pressure, or bearing down, leg fatigue, and low back pain.
- Urinary symptoms. Cystocele, urethrocele, and uterine prolapse can cause stress incontinence and difficulty in starting to urinate.
- Bowel symptoms. A rectocele may cause problems with defecation by forming a pocket just above the anal sphincter. Stool can become trapped, causing pain, pressure, and constipation.
- Sexual problems. A prolapse can cause irritated vaginal tissues or pain during intercourse, as well as psychological stress.
If you think you have a pelvic prolapse condition, contact us today. A traditional pelvic examination is the only way to diagnose it.
What do you need to know?
We have the ability to correct your pelvic organ prolapse with the latest techniques and the most minimally invasive approaches.